
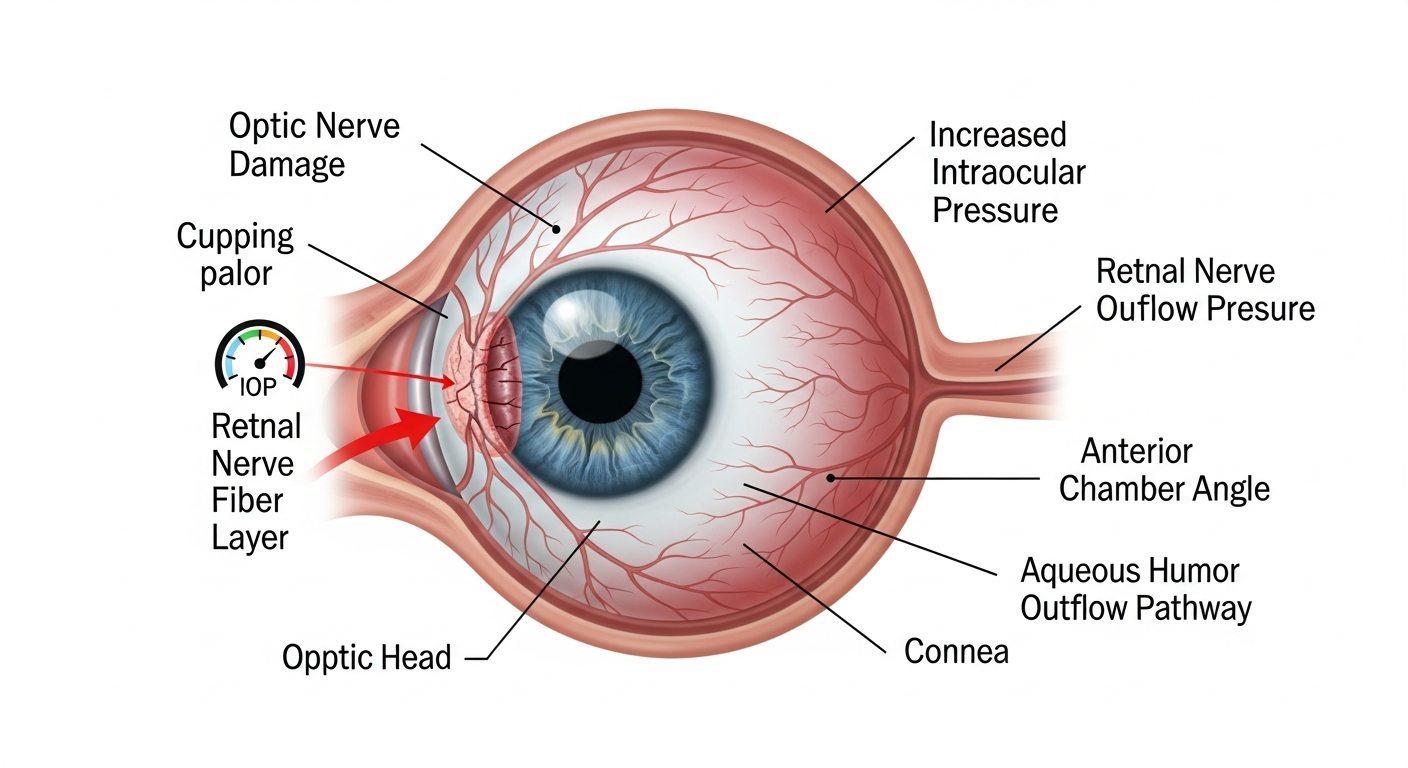
Glaucoma, a leading cause of blindness in the world, especially for older people. However visual loss is preventable or stabilized with early diagnosis and treatment. Glaucoma is a condition of the eye where the optic nerve is damaged. The optic nerve carries images to the brain, which are then perceived as vision. Minute nerve fibres from various parts of the retina join to form the optic nerve. Glaucoma results when the pressure within the eye is high enough to be detrimental to the normal functioning of these nerve fibres, some of which stop functioning. Non-functional nerve fibres result in a loss of retinal function in the area from where they originate, leading to defects in the field of vision. The disease is called the ‘sneak thief of sight’ because it is painless, without symptoms and irreversible. Therefore, the person with glaucoma is usually unaware of it until much loss of vision has occurred. In fact, half of those suffering damage from glaucoma do not know it. Currently, damage from glaucoma cannot be reversed and if the entire nerve is damaged, blindness results. Early detection and regular treatment are the keys to preventing optic nerve damage and blindness from glaucoma.
The aqueous humour is the clear fluid circulating within and nourishing some parts of the eye which have no blood supply. ‘Normal’ individuals have an equal production and drainage of this fluid resulting in a constant pressure within the eye. If the drainage is compromised due to any reason, there is a pressure build-up in the eye, which can damage the optic nerve.
Regular eye examinations by the ophthalmologist leads to detection.
The complete and painless examination includes (among other tests):
- Tonometry – Measurement of intraocular pressure
- Gonioscopy – Inspection of drainage angle of the eye
- Ophthalmoscopy – Evaluation of optic nerve damage
- Perimetry – Testing the visual field of each eye
- GDXVCC – Retinal nerve fiber layer analyser
- OCT – Retinal nerve fiber thickness and optic cup–disc size
People with high pressures have greater risk. Advancing age, high myopia, family history, diabetes, past injuries, surgeries, anaemia, or shock increase risk. High risk with no optic nerve damage: monitored as 'glaucoma suspect.'
Regular eye examination by an ophthalmologist is the best way to detect glaucoma. During a complete work up for glaucoma, your ophthalmologist will measure the intraocular pressure (tonometry), inspect the drainage angle of the eye (gonioscopy), evaluate for optic nerve damage (ophthalmoscopy), and test the visual field of each eye (perimetry). These tests must be repeated regularly to monitor the progress of disease.
Glaucoma can't be cured, but can be controlled and further damage slowed/halted. Requires lifelong treatment and regular checkups.