
Retina is the light sensitive inner layer of the eye where the images are formed and are later relayed to the brain. This is akin to the photographic film of a camera, and is very important for vision. Retinal detachment is a condition in which the Retina separates from the underlying layer and hence loses its functional capacity. A retinal detachment, leads to a sudden and severe loss of vision, and if not treated properly can cause blindness.
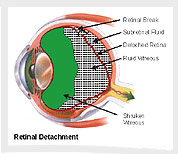 Rhegmatogenous Retinal Detachment is the most commonly seen type of detachment. In this form Retinal detachment occurs due to a hole/tear (Rhegma) formation in the retina. Through this hole, liquefied vitreous, which is jelly like substance filling the eyeball, passes behind the retina and detaches it.Tractional retinal detachment usually occurs in diabetics or other vascular diseases of the retina. Extensive membranes are formed on the retina, which on contracting, exert traction & hence pull the retina up resulting in Tractional Retinal Detachment.
Rhegmatogenous Retinal Detachment is the most commonly seen type of detachment. In this form Retinal detachment occurs due to a hole/tear (Rhegma) formation in the retina. Through this hole, liquefied vitreous, which is jelly like substance filling the eyeball, passes behind the retina and detaches it.Tractional retinal detachment usually occurs in diabetics or other vascular diseases of the retina. Extensive membranes are formed on the retina, which on contracting, exert traction & hence pull the retina up resulting in Tractional Retinal Detachment.
Presence of high degrees of myopia (minus power), injury to the eye, occurrence of retinal detachment in the fellow eye, occurrence of retinal detachment in the blood relatives, etc. are some of the factors that increase the risk of retinal detachment.
If one has any of the above mentioned risk factors, he/she should get regular retinal checkups. The pupils are dilated and the retina, is checked thoroughly with the help of Indirect Ophthalmoscope. In case a retinal break or lesion is discovered, it can be treated by a simple preventive procedure of Laser or Cryopexy.
Direct injury to the eye can lead to retinal breaks, holes, or tears that may cause retinal detachment days, weeks, months, or even years after the incident. Therefore, every patient with significant eye injury must get a detailed retinal checkup after the injury, and thereafter at regular intervals to detect these possible retinal breaks.
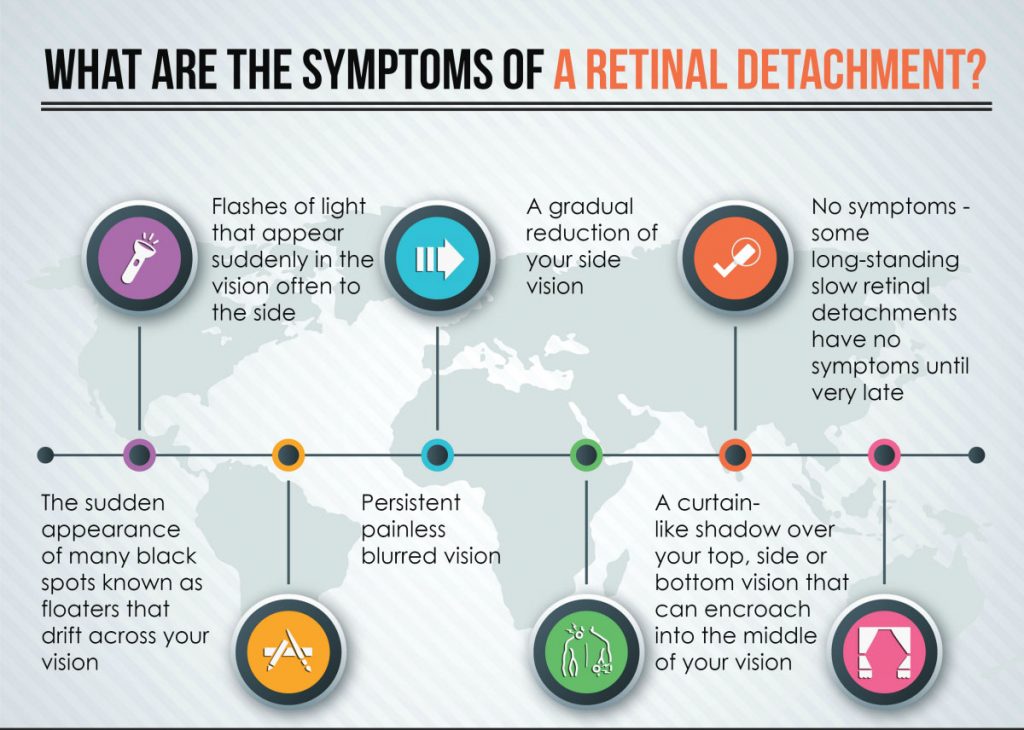
Perception of Flashes of light, or sudden onset of Floaters are common symptoms which may point towards the presence of a Retinal Tear or Retinal Detachment. However these two symptoms are also seen when vitreous detaches spontaneously or after trauma without Retinal Detachment. A loss of field of vision or sudden decrease in central vision is also complained by majority of patients with Retinal Detachment. The diagnosis is confirmed by a detailed retinal checkup by a retinal specialist. In case of poor visibility, B-scan Ultrasound test may be required to confirm the diagnosis.
When the retina stays detached for a long time, it starts to shrink and membranes form on it. This not only requires a major surgery, it also decreases the chances of success. Moreover, longer the retina stays detached, lesser is the visual gain after surgery. What is the treatment? A retinal tear without a detachment can be treated by a simple Laser or Cryopexy procedure. However a retinal detachment requires a major surgery to reattach the retina. Depending upon the severity of the case and other factors, one of the two options are generally used:
-
Retinal surgery
In selected cases, surgery called Scleral buckling is done, where a silicon plastic is placed on the outside of the eye and sewn in place (the scleral buckle is very small and not visible after surgery). It pushes the sclera toward the tear in the retina and closes it to settle the retina. Vitreo-Retinal Surgery
In more severe or advanced cases, along with Scleral buckling, vitrectomy may be necessary. In this procedure, the vitreous gel is removed using special instruments, and then retina is settled in place and is fixed there with the help of laser. To support the retina either Silicone oil or special Gas is injected in the eye to replace the vitreous. This injected oil is inert in nature and is generally removed later at a suitable time after the initial surgery, where as if gas is used it gets absorbed spontaneously after few weeks.
Post-operatively, the patient is asked to maintain a special position for few days to weeks to support the retina. This is especially required in cases of Vitreo-retinal surgeries. During the follow up visits, supplementary laser treatments may be also be done. As it is a major surgery, some of the patients may also develop complications like glaucoma, cataract, infection, corneal opacity etc. due to the detachment or due to the treatment. The fellow eye is also at a risk for future retinal detachment and must be checked at regular intervals. Hence a regular follow up is very important.
The primary aim of the surgery is to re-attach the retina. The vision regained primarily depends upon the ‘strength’ of retina, which in turn depends upon many factors, especially the duration of detachment. The earlier the surgery is done, the better are the visual results. The vision regained may not be the same as that before the detachment occurred. But in case no surgery is done, the vision is likely to deteriorate further leading to blindness, shrinking and disfiguration of eyeball. Hence it is important to do the surgery as soon as possible.
In some patients re-detachment may occur due to formation of membranes on the retina (called Proliferative Vitreo Retinopathy). Also in 20-30% of patients operated for Vitreoretinal surgery, retinal detachment may recur after the removal of Silicone Oil. Hence the patients are required to maintain regular post-operative follow up for a long time even after the surgery.
