
Oculoplasty, Aesthetics And Oncology
 Ophthalmic plastic surgery or ‘Oculoplasty’ is the branch of ophthalmology that deals not only with the diseases of the eye, but also important structures around the eyes like eyelids, eyebrows, orbit and the tear system which are vital to the normal appearance and function of our eyes. Common conditions needing ophthalmic plastic surgery:
Ophthalmic plastic surgery or ‘Oculoplasty’ is the branch of ophthalmology that deals not only with the diseases of the eye, but also important structures around the eyes like eyelids, eyebrows, orbit and the tear system which are vital to the normal appearance and function of our eyes. Common conditions needing ophthalmic plastic surgery:
Reconstructive Surgery-
- Eyelid Lift (Blepharoplasty)


Excess upper eyelid skin hanging down over the eyelashes may interfere with vision.The droopiness of the eyelids leads to reflex forehead wrinkling, headache from forehead muscle contraction, and eye fatigue. A simple 30-minute operation by an oculoplastic surgeon remedies the problem by removing the excess skin. Though this surgery is more popular as a cosmetic eyelid surgery, it is frequently performed when excess eyelid skin interferes with vision. The result is a more youthful,rested appearance of the eyes, softening of wrinkle lines, and widening of visual fields for partially blocked vision.
Eyelid lift surgery is usually performed in patients aged 50 and above, although it can be done as early as the 20s or 30s for inherited traits.
In the upper eyelid, Blepharoplasty involves removal of upper eyelid skin and fat through an incision hidden within the crease of the eyelid. In the lower eyelid, minimal amount of excess and wrinkled skin can usually be treated with a chemical peel or laser skin resurfacing. Large amounts of extra lower eyelid skin may require an incision just below the eyelashes to remove the skin for effective treatment.
Eyelid Surgery is performed on an outpatient basis under local anesthesia and takes about 45 minutes for the upper or lower eyelids, or an hour and a half for both together. Discomfort is minimal. Stitches are removed in 5-7 days. Most patients are back to light work within a week. Minimal bruising may persist for 1-2 weeks.
Notes:Excess eyelid skin may be a sign of drooping eyebrows, in which case a browlift is the preferred treatment. In addition, many patients with concerns of lower eyelid bags actually have a sunken appearance and would benefit from Fat transfer to fill in the lower eyelid area, rather than fat removal.
- Entropion

The in-turning of the eyelid causing the eyelashes to rub against the eye is called entropion. It can affect upper or lower eyelid, and is caused by laxity of the eyelid tissues, chemical injury, or eye surface disorders and may produce tearing, infection, vision impairment, and damage to the cornea. Repair of the supporting structures of the eyelid by an Oculoplastic surgeon can correct this problem.
n the upper eyelid, surgery involves incision on the back surface of the eyelid to correct the inturning, and allow it to heal in an out-turned manner with the help of temporary sutures. In the lower eyelid, it is commonly caused due to aging and laxity of tissues, and needs simple tightening of the supporting structures of the eyelids (retractors).
Eyelid Surgery is performed on an outpatient basis under local anesthesia and takes about 45 minutes. Discomfort is minimal, and stitches are removed in 7-14 days. Most patients are back to light work within a week. Minimal bruising may persist for 1-2 weeks.
Notes:Severe cases with history of past surgeries may need mucous membrane graft (taken from the inside of your cheek or lip), cartilage graft or more complex eyelid reconstructive procedures. Despite a successful surgery, occasional abnormal lash might require removal by electrolysis. Entropion surgery may be combined with mucous membrane graft, amniotic membrane graft, electrolysis, or complex eyelid reconstruction in severe cases.
- Ectropion

Out-turning of the eyelid is called ectropion, and can lead to redness, irritation, watery eyes, infection, crusting, vision impairment, and damage to the cornea (surface of the eye). This almost always affects the lower eyelid only, and can result from facial aging, injury, tumor, or Bell’s Palsy. Repair of the supporting structures of the eyelid by an oculoplastic surgeon easily corrects this problem.
The out-turned lower eyelid and the lax tissues need simple tightening of the supporting structures, performed through a small incision at the outer corner of the eyelids (Lateral canthoplasty).
Eyelid Surgery is performed on an outpatient basis under local anesthesia and takes about 45 minutes. Discomfort is minimal, and stitches are removed in 5-7 days. Most patients are back to light work within a week. Minimal bruising may persist for 1-2 weeks.
Caution:Severe cases of Bells Palsy may need additional medial canthoplasty, or supporting fat grafting in the lower eyelid. Ectropion surgery may be combined with medial canthoplasty, or lower eyelid dermis fat graft. Severe cicatricial ectropion resu;ting from trauma or burn etc may need larger reconstructive surgeries like skin graft or complex eyelid reconstruction.
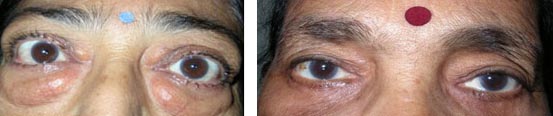
- Eyelid Drooping (Ptosis)
 Droopiness (ptosis) or sagging of the upper eyelid can occur as a result of birth defect, injury, muscle disorder, nerve disorder, or simply due to aging. It can obstruct vision when severe, and create a tired, aged or sleepy appearance. Eyelid ptosis may also cause excessive forehead wrinkling, headaches from forehead muscle contraction,abnormal head posture such as chin elevation to improve vision, and eye fatigue. When it is present since birth, severe droop might obstruct development of vision leading to a lazy (amblyopic) eye with subnormal vision. Thus, correction of drooping is of functional importance in children, and a functional as well as cosmetic concern in adults. Surgery can correct this problem by repairing the muscle and supporting the eyelid. Several surgical options are available, and the type of surgery used depends upon the severity of the droop.
Droopiness (ptosis) or sagging of the upper eyelid can occur as a result of birth defect, injury, muscle disorder, nerve disorder, or simply due to aging. It can obstruct vision when severe, and create a tired, aged or sleepy appearance. Eyelid ptosis may also cause excessive forehead wrinkling, headaches from forehead muscle contraction,abnormal head posture such as chin elevation to improve vision, and eye fatigue. When it is present since birth, severe droop might obstruct development of vision leading to a lazy (amblyopic) eye with subnormal vision. Thus, correction of drooping is of functional importance in children, and a functional as well as cosmetic concern in adults. Surgery can correct this problem by repairing the muscle and supporting the eyelid. Several surgical options are available, and the type of surgery used depends upon the severity of the droop.
When the eyelid droop is mild, a simple tightening of the eyelid lifting muscle (levator) performed from the back of the eyelid (Mullerectomy) is needed. There is no skin scar in this surgery.
Moderate droop requires tightening of the muscle that lifts the eyelid (levator), and is preferably done via skin incision that is typically hidden in the upper eyelid skin fold.
In severe droop, tightening the eyelid muscle does not help. In that case, the eyelid has to be connected to the brow elevating muscle (frontalis) to effect eyelid lift. This surgery (called tarso-frontal sling surgery) can be preformed using various sling materials, and involves small (2-3mm) stab incisions over the eyelid and just above the brow. Sling surgeries are generally not permanent, and the eyelid often droops in a few years due to blinking and gravity, which act against the upward lift. A patient of sling surgery may therefore need multiple revisions of the surgery over his/her lifetime, possible through the same initial stab incisions.
Surgery for mild to moderate droop can be performed on an outpatient basis under local anesthesia and takes about 30 to 45 minutes. Discomfort is minimal, and stitches are removed in 5-7 days. Most patients are back to light work within a week. Minimal bruising may persist for 1-2 weeks. For severe ptosis (sling surgery) and for children, general anaesthesia is needed therefore necessitating a day’s admission.
Notes:Often times, ptosis surgery needs one or two sessions of suture adjustment (1-6 weeks after surgery) to match it to the other eye. 0.5 mm to 1 mm error remains in some severe cases, which is generally cosmetically well accepted. In case of severe ptosis, correction is optimal only in straight gaze. The eye appears slightly droopy in upgaze, and slightly wider in downgaze. Closure may also be incomplete, especially during sleep. Ptosis surgery may also be combined with upper eyelid blepharoplasty or lower eyelid blepharoplasty.
- Eyelid and Skin Cancer Reconstruction

Skin cancers can involve the face or the eyelids. In India, sebaceous gland carcinoma is the most common type of skin cancer involving the eyelids. It usually presents as an elevated nodule with yellowish nodules within. There are fine blood vessels on the surface. Other less common tumors are basal cell carcinoma and squamous cell carcinoma.
 Most skin cancers are painless nodules, sometimes pigmented, and may bleed occasionally. They rarely spread to other regions of the body, and are usually not life threatening. When the cancer is removed and the region is reconstructed, the patient is essentially cured. There is a 5% or less chance that the cancer may recur, hence periodic check-up is needed.
Most skin cancers are painless nodules, sometimes pigmented, and may bleed occasionally. They rarely spread to other regions of the body, and are usually not life threatening. When the cancer is removed and the region is reconstructed, the patient is essentially cured. There is a 5% or less chance that the cancer may recur, hence periodic check-up is needed.
Management of any eyelid or skin cancer involves two major steps: complete removal, and subsequent reconstruction. Currently, histopathological confirmation during surgery (Frozen section) is the best method to ensure complete removal of the tumor. Reconstruction of the face after removal of the cancer is dependent on the size and location of the defect. Flaps, skin grafts and other options are available. A flap is a technique whereby adjacent skin is rotated into the deficient area. Skin grafts (taken from behind the ear or opposite eyelid) are also sometimes used to reconstruct the defects. Ideally, the skin graft should match in color and complexion. Occasionally, eyelid-sharing procedures are needed which are done in 2 stages performed 6-8 weeks apart.
Surgery for eyelid cancers vary widely in their complexity and duration based on the location and extent of the tumor. Small tumors can be removed under local anesthesia and take about 1-3 hours including reconstruction time. More often, general anesthesia is preferred. Stitches are removed in 7-10 days. Most patients are back to light work within a week or two. Minimal bruising may persist for 1-2 weeks.
Notes:Cancer surgery may need skin graft, cartilage graft, and complex periocular flaps as a part of the reconstruction. Extensive eyelid tumors involve permanent loss of lashes after reconstruction. Recurrence though rare is possible, either within the original site or within a draining lymph node (around the ears, jawline and neck). Extensive tumors spreading into the orbit may need simultaneous removal of the eyeball, even if vision seems to be good.
- Facial Spasms (Eyelid Spasm) and Botulinum Toxin
The muscles of facial expression and the eyelid are normally under our voluntary control. Facial spasm is a condition in which these muscles function abnormally and are no longer under the direct control of the brain. It can affect either one small area of the face, or the entire face including the neck.
Benign Essential Blepharospasm (BEB) is caused by an uncontrolled nerve signal in the brain that stimulates the eyelid muscles. Constant involuntary blinking and squeezing of the eyelids causes visual interruptions in the patient’s day to day activities. Hemifacial spasm (HFS) is commonly caused by an irritation of facial nerve on one side, leading to involuntary spasms on one half of the face. Meige syndrome involves spasms over the entire face. Myokimia is a more localized form of spasm, that typically involves a single eyelid or periocular area. Botunlinum toxin injection (BOTOX) into the eyelid muscles can significantly reduce the muscle spasm that causes contraction or twitching of the eyelids.
Injection procedure is performed as an out patient procedure, and takes 10 minutes. Application of local anesthesia cream an hour before the procedure makes it almost painless. The effect takes 7-10 days, and can last for 3-4 months.
Notes:Botulinum toxin controls the spasm, and does not treat it. Therefore, repeated injections are required for continued effect. Some patients may be non-responsive to Botox, and would need surgical correction of spasm.
- Surgery for a Watering Eye
Watery eye is usually a sign of blocked tear ducts resulting from infection, injury, or rarely a tumor. Tear duct surgery may be performed to open or bypass the duct and allow the tears to drain directly into the nose (Dacryocystorhinostomy, or simply DCR). Tear duct surgery can be performed through a small incision in the corner of the eye or with endoscopic surgery (with a tiny microscope) through the nose. When tear duct is blocked since birth (due to non-canalization), it can lead to watering since birth.
Surgical Time and Recovery:
DCR surgery is performed as an inpatient procedure under general or local anesthesia and takes about 45 minutes. Discomfort is minimal after surgery, and lasts for a week. Stitches are removed in 5-7 days. Most patients are back to light work within a week. Probing procedure is performed when tear duct is blocked since birth. It is performed as a short out-patient procedure, and does not leave any external scar.
Note:DCR performed through the nose (endonasal) can avoid a scar, but also has a slightly lower success rate as compared to the external approach. Along with DCR, additional procedures like silicone intubation, and the use of anti-scarring medicines like Mitomycin-C may be used to increase the success rate of the procedure. Bleeding is usually encountered in this type of surgery; therefore the patient should have controlled blood pressure. In case patient is taking blood thinners like Aspirin then it should be stopped for at least 3 days before surgery in consultation with his cardiologist. Not all tear duct blocks can be treated with DCR. Some require addition placement of silicone tubes, and others need a different bypass called a Jones tube.
- Thyroid Eye Disease
Thyroid eye disease (a condition of Graves’ disease or hyperthyroidism) causes the eyes to bulge forward and the eye aperture (gap between two eyelids) to widen. This leads to double vision, severe inflammation, discomfort, dry or watery eyes, corneal abrasions, infections, and possibly loss of vision. The initial (active) phase of thyroid eye disease involves frequent swelling of tissues around the eyes, double vision, and even reduction in vision in severe cases. Active phase is treated with medications to reduce the swelling. Fortunately, the active phase of most thyroid eye disease patients ends in 18-24 months. However, the deformities (raised eyelid, prominent eyeball, or squint) may persist, and now requires surgery.
Surgical Time and Recovery:
Decompression surgery is typically performed first in the staged surgical management of thyroid eye disease. It involves expanding the bones of the eye socket to allow the eye to fall back. It can be performed under local or general anaesthesia depending upon the severity. Muscle surgery is performed next to alleviate double vision if present. Eyelid surgery is often the last stage of rehabilitation whereby the eyelids are lowered, yielding a more natural, aesthetically pleasing appearance and reducing the chance of future eye-related complications. Discomfort is controlled with medications after surgery, and lasts for a week. Stitches are removed in 5-7 days. Most patients are back to light work within a week.
Note:Multiple procedures are often required to bring the patient to a near normal appearance, and one has to wait for the active phase to pass away before surgery can be performed.
Orbital Surgery
The Orbit (eye and surrounding bones) can be adversely affected by the presence of a tumor. The tumor could produce forward protrusion of the eye, reduce vision due to compression upon the nerve, or cause double vision. Most orbital tumors are benign (non-cancerous), however, some can be malignant (cancerous), especially in the elderly. Appropriate management of such cases needs a CT scan or MRI imaging followed by complete removal or partial (diagnostic) biopsy of the tumor.
Surgical Time and Recovery:
In most situations, it is possible to remove the tumor by performing a surgery called orbitotomy. The surgery is performed through an incision that is hidden behind the eyelid or within the upper lid fold. Eyeball function is preserved. In severe cases however, it is sometimes necessary to remove the eye completely. It can be performed under local or general anaesthesia, depending upon the location of the tumor, and can take anything from 45 minutes to 3 hours. Discomfort is controlled with medications after surgery, and lasts for a week. Stitches are removed in 5-7 days. Most patients are back to light work within a week
Note:It is not possible to remove all tumors completely, especially when there is a suspicion of cancer. A small biopsy (incisional biopsy) is performed for diagnosis, and remaining tumor is treated with medications or radiation based on final pathology diagnosis. Mostly the eyeball function is preserved but in very few circumstances patient may have temporary or permanent double vision, ptosis, decreased vision etc..(it varies depending upon case to case basis).
- Trauma and Maxillofacial Surgery
Trauma can affect any structure of the eyelid, eyeball and the surrounding bones (fracture) depending upon the mechanism and force of injury. Laceration of the eyelid needs meticulous placement of stitches to preserve its normal shape and function. Injury to the tear ducts (canaliculus) within the eyelids require special placement of silicone tubes within them to keep them open while the injured eyelid heals. A thorough examination is also done to find out if the eyeball is also injured. Fractures of the bone surrounding the eye (orbital walls) may cause the eye to sink back into its socket, lead to a facial deformity, poor eye movement, or loss of vision. A clinical examination combined with a CT scan of the orbit can easily detect any of this possibility. The presence of any retained foreign bodies also needs to be ruled out. Orbital fractures can now be repaired with minimal incisions through the inside of the eyelid or mouth. Most often, a barrier has to be placed to cover the fracture site. Excellent synthetic plates (polyethylene or silastic) are available for this purpose, or alternatively a small sliver of patient’s own bone can be safely removed from elsewhere and placed over the fracture site.
Surgical Time and Recovery:
Eyelid laceration repair can be performed under local or general anesthesia, depending upon the location and extent of the injury. Fracture repair almost always requires general anesthesia. Trauma repair can take anything from 30 minutes to 3 hours. Discomfort is controlled with medications after surgery, and lasts for a week. Stitches are removed in 5-7 days. Most patients are back to light work within a week.
Caution: The outcome of trauma repair entirely depends upon extent and severity of injury. Healing often continues for months, and treatment has to be modified according to the course of healing.
- Pterygium
Pterygium (pronounced “tur-RIDGE-ium”) is a benign thickening of the outer coating (conjunctiva) of the eye that grows onto the cornea. As a pterygium grows, it may become red and irritated. Eventually, it may cause visual disturbances by disrupting the normally smooth surface of the cornea. In severe cases, a pterygium can block a patient’s vision altogether. No-stitch pterygium surgery is made possible by the use of modern tissue adhesive*, composed of clotting proteins normally found in human blood. Tissue adhesive allows the surgeon to secure a conjunctival autograft in seconds rather than minutes. After about one week the tissue adhesive dissolves, leaving no residue, and the eye heals comfortably.
Causes of Pterygium
UV radiation (usually from sunlight) is the most common cause of pterygium. This explains why pterygium occurs with increasing frequency in climates approaching the equator. Other causes include continuous exposure to dry, dusty environments. People who spend significant time in water sports (surfing or fishing) are particularly susceptible to pterygium because of the intense exposure to UV that occurs in these environments. When the eye is continuously assaulted by UV rays, the conjunctiva may thicken in a process similar to callus formation on the skin. The sensitive structures of the outer eye often can not comfortably tolerate this degenerative process, and irritation, redness, foreign body sensation, and ocular fatigue can result.
Preventing Pterygium
The best method of preventing pterygium is to regularly wear UV 400 rated sunglasses when outdoors in sunny conditions. Sunglasses with a wrap-around design provide better protection than those with large gaps between the sunglass frame and the skin around the eyes. Wearing a hat with a wide brim provides valuable additional protection.
Treating Pterygium
In mild cases, pterygium redness and discomfort can be controlled with lubricant eye drops (artificial tears). When symptoms of redness, irritation, or blurred vision are resistant to conservative treatment, or when vision is affected by progressive growth of a pterygium, surgery is considered
History of Pterygium Removal Surgery
In pterygium surgery, the abnormal tissue is removed from the cornea and sclera (white of the eye). Over the years, pterygium surgery has evolved significantly, and modern pterygium surgery has a significantly higher success rate than conventional surgery. In traditional “bare sclera” pterygium removal, the underlying white of the eye (sclera) is left exposed. Healing occurs over two to four weeks with mild to moderate discomfort. Unfortunately, the pterygium may grow back in up to 50% of patients. In many cases, the pterygium grows back larger than its original size. Traditional “bare sclera” pterygium surgery has a high rate of re-growth. Occasionally, the pterygium grows back larger than the original. Over the years, surgeons have used several different techniques to lessen the likelihood of pterygium recurrence, including radiation treatment and the use of “antimetabolite” chemicals that prevent growth of tissue. Each of these techniques has risks that potentially threaten the health of the eye after surgery, including persistent epithelial defects (ulceration in the surface of the eye), and corneal melting.
Conjunctival Autograft with Stitches
Most cornea specialists today perform pterygium surgery with a conjunctival autograft because of a reduced risk of recurrence. In this technique, the pterygium is removed, and the cornea regains clarity. However, the gap in the mucous membrane (conjunctiva) tissue, where the pterygium was removed, is filled with a transplant of tissue that has been painlessly removed from underneath the upper eyelid. Although the procedure requires more surgical skill than traditional surgery, this “auto-graft” (self-transplant) helps prevent re-growth of the pterygium by filling the space where abnormal tissue would have re-grown. In conventional autograft surgery, stitches are used to secure the graft in place on the eye. These can cause discomfort for several weeks. The autograft is held in place with tiny stitches that may dissolve after a few weeks or can be removed in the surgeon’s office. Stitches on the eye frequently cause discomfort, however, after pterygium/autograft surgery. The desire for a quicker, more painless recovery has led to the development of no-stitch pterygium/autograft surgery.
No-stitch Pterygium/Autograft Surgery*
No-stitch pterygium/autograft surgery allows most patients to return to work within one or two days of surgery. A research study on 85 patients with pterygium conducted at Harvard Eye Associates has shown that patients undergoing no-stitch surgery had significantly less pain after surgery than those having traditional surgery. The no-stitch technique also reduced surgery time from an average of 21 minutes to 14 minutes. No pterygium recurrences were found in any patients in the study.
Technique for No-stitch Pterygium/Autograft Surgery
In no-stitch surgery, the patient is lightly sedated to ensure comfort, and the eye is completely numbed, so there is no way to see the surgery occurring and no sensation of discomfort. The abnormal corneal tissue is removed and replaced with a thin graft of normal tissue. Over the next 2-3 weeks, the eye gradually returns to a normal appearance.
