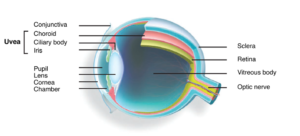
The eye is an important sense organ. It is made up of 3 coats. The outer coat is the cornea and sclera. The middle coat is the uveal tract and the inner coat is the retina. The uveal tract consists of 3 parts. The iris is the visible part of the uvea and gives color to the eye (blue, black, brown). The ciliary body is the middle layer of the uvea which manufactures the fluid inside the eye. The choroid is the posterior layer of the uvea which is rich in blood vessels.
Inflammation or swelling in any of the part of the uveal tract is called uveitis. Depending on the location of inflammation, it is called anterior uveitis (iris and ciliary body is involved), intermediate uveitis (ciliary body and the vitreous is involved), posterior uveitis (choroids and retina involved), panuveitis (all layers of the uveal tract are involved).
Causes of uveitis are many.
- It may result from an infection (bacteria like tuberculosis, viruses like herpes, parasites like toxoplasmosis)
- It may also be related to an autoimmune disease (with or without involvement of other parts of the body). This essentially is when our immune system recognizes a part of our own body as foreign and elicits a reaction in the form of uveitis.
- The uveitis may be the presenting manifestation of an underlying systemic disease.
- It can occur as a result of injury to the eye.
- It can occur due to other disorders in the eye like cataract and retinal detachment
- Sometimes the cause is not known at the first instance. As we follow-up the patient over a period of time, we may be able to pick up new clues or signs suggestive of a systemic disease. In such cases, they are labeled as idiopathic (cause not known) at the initial visit.
Depending on the structure involved, the symptoms can vary from
- Pain
- Redness
- Inability to see light (photophobia)
- Black spots moving in front of the eye
- Blurring or reduction in vision
An initial examination of the eye will be done. This includes the recording of the visual acuity by reading a chart (to check if the vision has decreased), slit lamp examination; (in which a narrow beam of light is shone into the eye so that a magnifying lens can closely examine the highlighted portion of the eye). Intraocular pressure recording (a painless test done by a tonometer); fundus examination (in which the pupil is widened so that the ophthalmologist can look into the eye and see structures in the back of the eye).Because uveitis can be caused by so many different things (infections/autoimmune diseases) diagnosis may require detailed laboratory investigations and a referral to a uveitis specialist.
Uveitis is the 3rd leading cause of blindness. Inflammation of the uvea can affect the cornea, retina, sclera and other vital parts of the body. Inflammation inside the eye is a medical emergency because, untreated, it will lead to vision loss. Damage to the eye is preventable if detected early and treated adequately.
The treatment of uveitis aims to achieve the following:
- Relief of pain and discomfort (when present)
- To prevent sight loss due to the disease or its complications
- To treat the cause of the disease where possible.
Medical treatment of uveitis must be aggressive to prevent glaucoma, to prevent scarring of the structures inside the eye and to prevent possible blindness. Different medications are used to control the original cause of uveitis, if known and to minimize the inflammation itself. Eye drops especially steroids (to reduce inflammation and pain) and pupil dilators (to widen the pupil and relax the muscles within the eye) are the main medications used to treat uveitis. For deeper inflammations, oral medicines eye injections or intravenous injections of steroids may be necessary. More severe cases of uveitis and those intolerant to steroids may require treatment with immunosuppressive agents. Complications such as glaucoma, cataract or new blood vessel formation (neovascularization) also may need treatment in the course of the disease. If complications are advanced, conventional surgery or laser surgery may be necessary.
The duration of treatment varies from person to person and also depends on the type and cause of uveitis. Simple forms of uveitis, for example, may respond to treatment within days and may not recur. Chronic (long term, recurring) forms of uveitis that threaten vision can be very difficult to cure and require persistence on the part of the treating physician(s) and patient. The length of time required to get the disease into a durable remission on steroids or immunosuppressants is difficult to quantify and is very individualistic but a minimum of 2 years is a reasonable estimate. With appropriate, targeted treatment, most people with uveitis will become well controlled and progress to remission. Once in remission from uveitis, you should expect to have regular follow-up visits to our doctor to make sure that the disease remains in remission.
You have to help to save your sight.
Find support and encouragement from your family, friends and others. Sometimes it helps to talk to people who have experienced the same thing. It can help you to discuss side effects, share ways to remember your medicines and celebrate getting your uveitis under control. Unfortunately, there are a few people who might lose vision despite commitment to working with their eye doctor and following their treatment plan.
The future holds great promise for uveitis. New medicines and treatments continue to be developed. In the meantime, take heart in knowing that we are doing everything possible to treat your condition. The doctor/patient team approach, support from others and promising scientific discoveries will help you look forward towards a bright future.
